Internal Funding Opportunity
Technology Advancement Program
Internal Funding Opportunity
The SickKids Technology Advancement Program (TAP) advances late-stage pre-clinical health care innovations through project funding, structured advice, project governance, and strategic networking opportunities.
Bring your innovation to the next level.
The SickKids Technology Advancement Program (TAP) is an initiative led by the Industry Partnerships & Commercialization (IP&C) office to advance late-stage pre-clinical health care innovations through project funding, structured advice, project governance, and strategic networking opportunities. TAP strengthens IP&C’s ability to develop and de-risk SickKids innovations beyond basic proof-of-principle.
This initiative is supported by the SickKids Commercialization Advisory Board (CAB), a panel of experienced commercialization and investment professionals who provide tailored feedback and guidance to help refine each project’s pathway to impact. The CAB selects projects to receive up to $350,000 in funding to facilitate proposed de-risking and commercialization activities.
2026 Technology Advancement Program
Call for Expressions of Interest
IP&C is excited to open the call for Expressions of Interest (EOIs) for the 2026 Technology Advancement Program (TAP). As part of our growing continuum of commercialization support, TAP empowers SickKids innovators by advancing late-stage pre-clinical technologies through mentorship, strategic guidance, and development funding. We encourage researchers with high-potential discoveries and a clear vision for translation to submit an EOI and take the next step toward impact.
The deadline for EOI submissions has passed.
Invitations to apply will be sent on March 4, 2026.
2026 Program Guidelines
2025 Technology Advancement Program
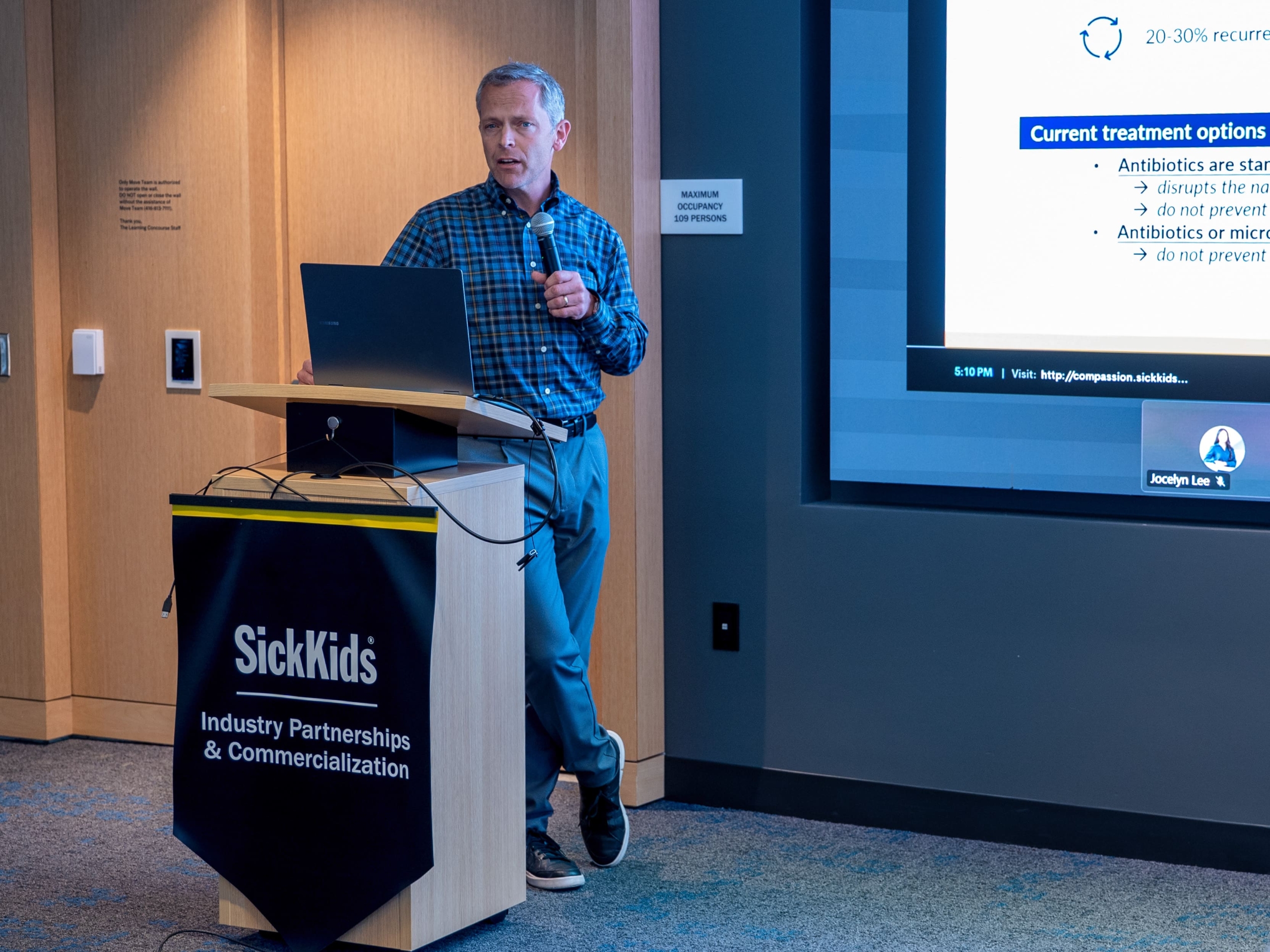
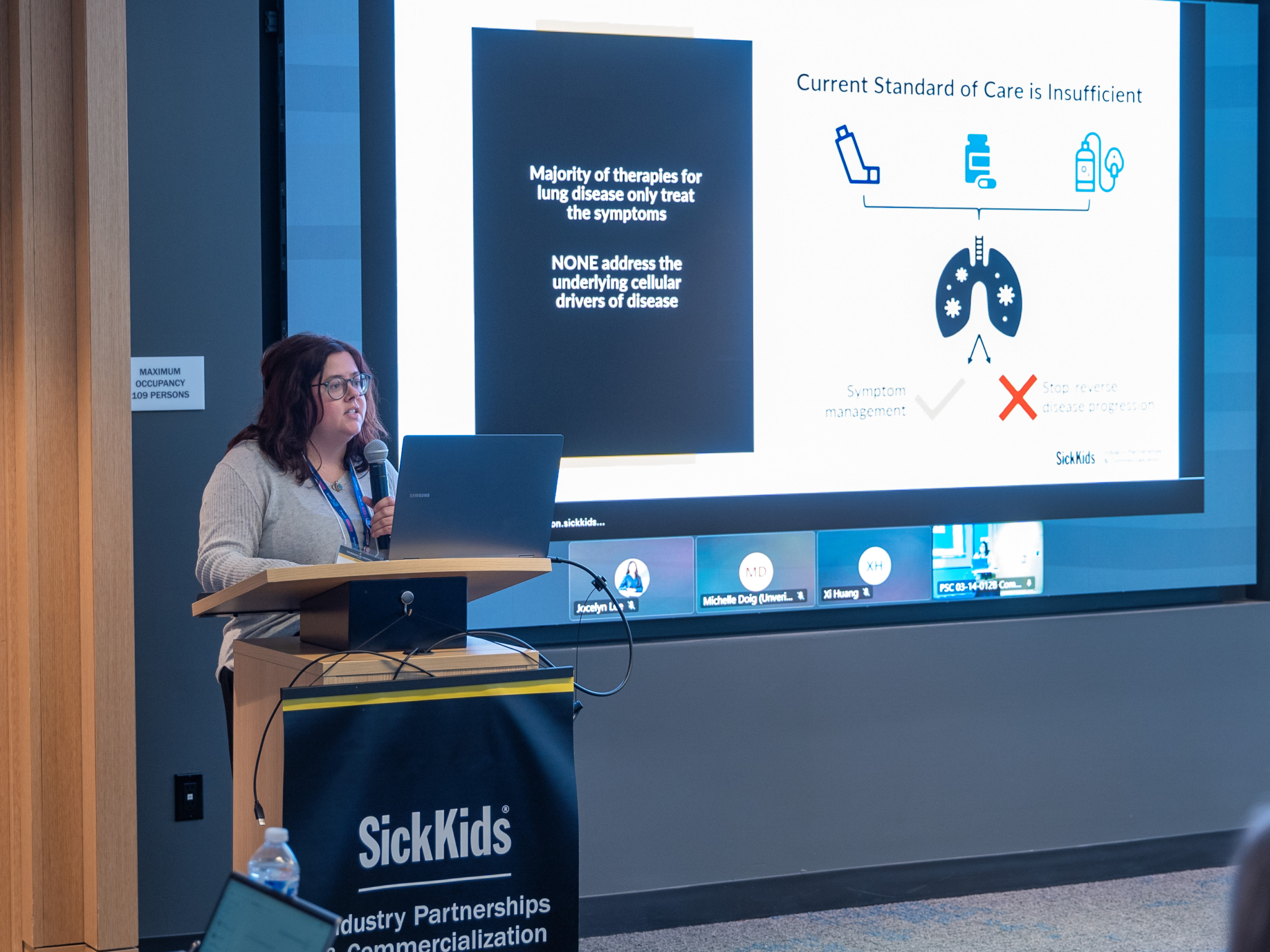
The inaugural SickKids Technology Advancement Program (TAP) ran from March to August 2025, supporting three promising projects with IP&C-led guidance and input from leaders in investment and industry. Projects selected to participate in the program addressed clearly defined clinical needs, demonstrated strong intellectual property positioning, and were at a stage where funding and mentorship could drive meaningful progress toward commercialization.
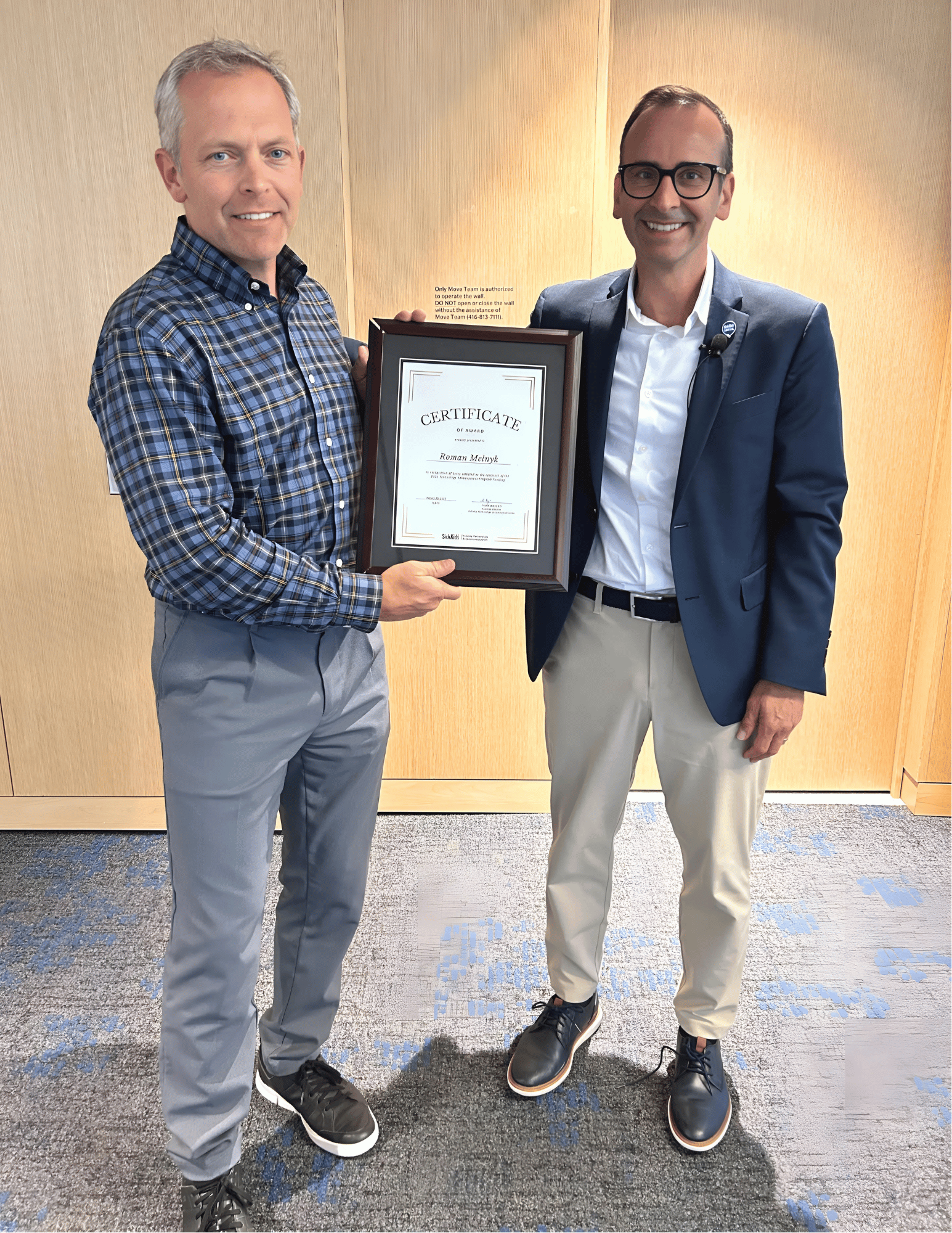
The program culminated on August 20, 2025, with final pitch presentations during which lead investigators showcased the scientific merit, market opportunity, and advancement potential of their innovations. Following thoughtful discussion and deliberation, the SickKids Commercialization Advisory Board (CAB) selected Dr. Roman Melnyk as the 2025 TAP funding recipient for his project aimed at mitigating Clostridioides difficile infections. His work will receive $350,000 in development funding along with continued mentorship to support future commercialization activities.